65 yr old male patient with sob and abdominal distension
C/O ABDOMINAL DISTENSION SINCE 1 1/2 MONTH
C/O B/L LOWER LIMB SWELLING SINCE 1 1/2 MONTH
C/O BREATHLESSNESS SINCE 1 MONTH
HOPI
A 65 yr potato chip vendor resident of bhongiri was brought to casualty on wheel chair on 20 /12/22 with complaint of abdominal distension since 1 1/2 month gradually progressive not associated with pain .H/o b/l lower limb swelling since 1 1/2 month gradually progressive associated with discharge of watery fluid
H/o breathless ness of grade 2 to 3 MMRC since a month insidious onset gradually progressive No H/
O chest pain / decreased urine output / PND/Orthopnea /fever/cough/ cold / breathless ness / day time sleepiness / .Now admitted for further management and treatment
Past history
Pt had breathless ness for which bought for consultation and diagnosed with HTN and DM 6 yrs back
He is on medication
1 t amlodipine 5 mg po/od at 8 am
2. T glimipiride 2 mg + met formin 1000 mg po/ od at 8 am
He is known case of CVA hemiplegia on rt side with deviation of mouth to left side 15 yrs ago ji
Got treatment for 5 yrs -resolved
H/o head injury 30 yrs ago in a train accident pt had injury at occipital region of scalp followed by altered behaviour for 6 months and used treatment for 6 months and resolved
H/o rt knee joint pain 5 yrs back
PERSONAL HISTORY:
Sleep - Decreased from 2 years
Diet - Mixed
Appetite - decreased
Bowel and bladder movements : regular
Addictions : Alcoholic
Started at 17 yrs daily 160 ml brandy till sep 2022 from 1 St oct 90ml
Tobacco
Started at 17 yrs 36 beedis / day till sep 22
Daily 1 beedi / day from 1 St oct
Treatment history
Blood transfusion 5 months ago
Drug history
T etophylline and T theophylline po/hs. Since 5 days
General examination
Pt. is conscious , coherent , cooperative
Vitals
BP 140/90 mmhg
PR 90bpm RR 18
GRBS. 114 spo 2 95
Pallor - absent
Icterus - absent
Cyanosis - absent
Clubbing - present
Lymphadenopathy : absent
Edema : Present till knee level and of pitting type
Per ABDOMINAL examination
INSPECTION
Abdomen is DISTENDED with flanks full
umbilicus is central slit like
Peude orange type of skin
No scars and sinuses
No ENGORGED veins
No visible pulsation
PALPATION :
all inspectory findings confirmed
No rise of temperature and tenderness
No guarding and rigidity
Organomegaly not able to elicit
Abdominal girth was127cms
At present 125 cms at umbilicus
Weight was 100kg
PERCUSSION :
Shifting dullness - Present
Fluid thrills - negative
Puddle sign cannot be elicited ,as pt is not cooperative
:Abdominal girth 127 now 125 at umbilicus
Weight was 100kg
AUSCULTATION :
bowel sounds are heard
No bruits
CVS
S1S2 +, no murmurs
Respiratory system
BAE + with b/l Ronchi
CNS
HMF intact
Power u/ l l/l
Rt. 5/5. 5/5
Lt. 5/5. 5/5
Reflexes.
Rt. Lt
Biceps. ++. ++
Triceps. +. +
Supinat. +. +
Knee. _. Ve. _ Ve
Ankle. _ Ve. _. Ve
Plantar. F. F
No cerebellar and meningial signs
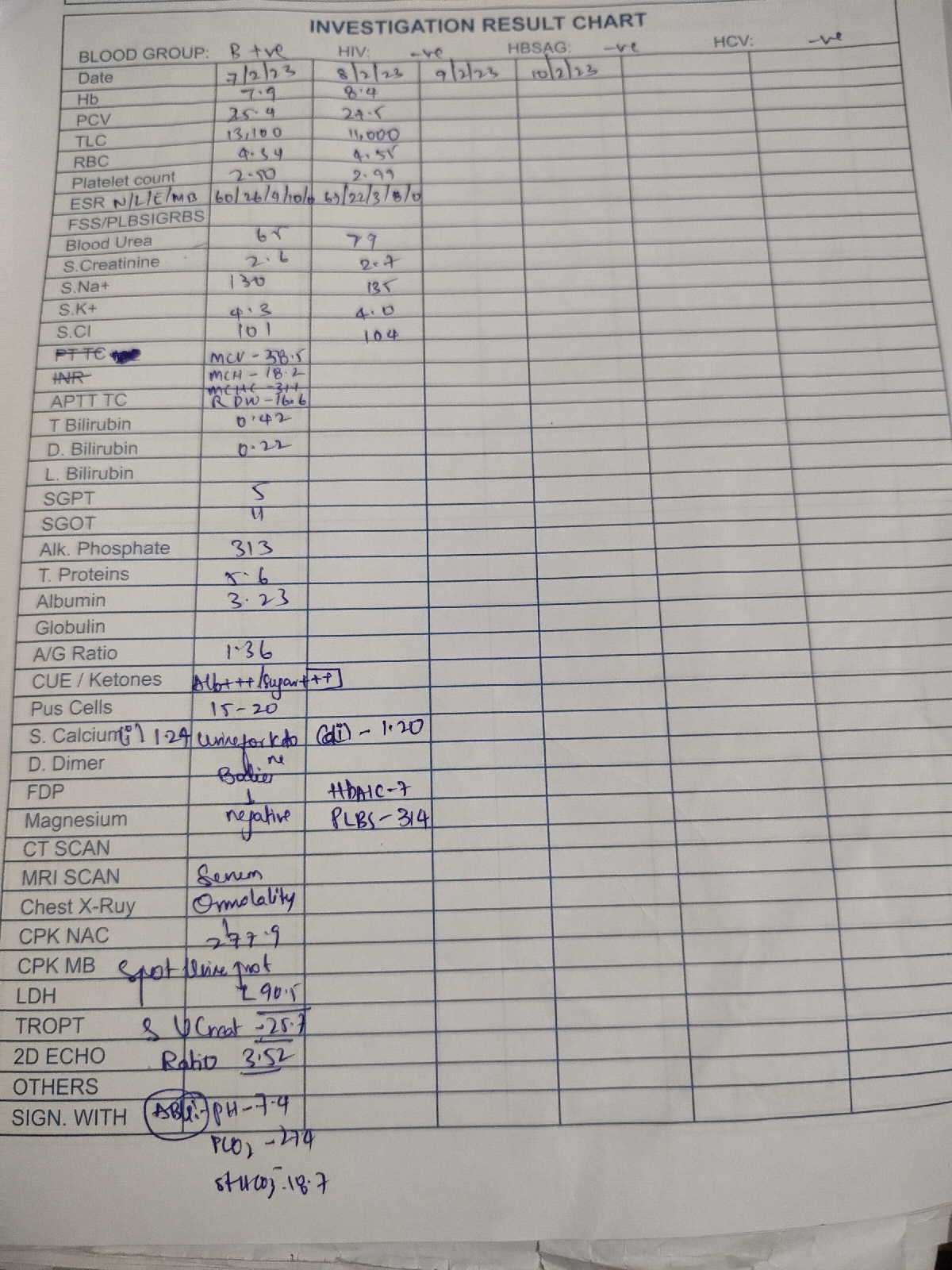
INVESTIGATION S
Urine culture and sensitivity
No pus cells and polymicrobial flora grown
Ascitic fluid cytology
No cells seen
Ascitic culture and sensitivity
No acid fast bacilli
No pus cells and organism seen
X ray
Ecg
Ultrasound abdomen
Gall bladder edema
Liver. Coarse echotextire with irregular surface
So chronic liver disease
No IHBRD
Gross ascites
Diagnosis
CHRONIC DECOMPENSATED LIVER DISEASE WITH HIGH SAAG LOW PROTEIN ASCITES SECONDARY
TO ALCOHOLIC LIVER DISEASE WITH B/L LOWER LIMB EDEMA GRADE 2 WITH HYPONATREMIA AND HYPOKALEMIA
Treatment
1 Inj. Lasix 40mg iv/od
2 T. Aldactone 50mg po/od
3 Syp. Lactulose 15ml po/tid
4 Inj HAI s/c acc. To grbs
5. Tab. Amlong 5mg po/od
6. Fluid restriction < 1.5L/day
7. Salt restriction < 2 g/day
8 Therapeutic paracentesis
Soap notes
ICU bed no 4
S
Sob in lying down position
Stools passed
No fever spikes
O
O/e
Pt. is c/c/c
BP 140/90 mmhg
PR 90bpm RR 18
GRBS. 114 spo 2 95
CVS S1S2 +
RS BAE + with b/l Ronchi
P/A distended
CNS HMF intact
-A
Decompensated chronic liver disease(secondary to alcohol)
with known case of diabetes and Hypertension
P
1 Inj. Lasix 40mg iv/od
2 T. Aldactone 50mg po/od
3 Syp. Lactulose 15ml po/tid
4 Inj HAI s/c acc. To grbs
5. Tab. Amlong 5mg po/od
6. Fluid restriction < 1.5L/day
7. Salt restriction < 2 g/day
8 Therapeutic paracentesis
-
-