This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs". This E log book also reflects my patient-centred online learning portfolio and your valuable comments on comment box is welcome.
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
Name K Santosh Kumar
Roll no 52
CASE DETAILS
An 80yr old male patient hailing from rural nalgonda a known case of CHRONIC KIDNEY DISEASE ON DIALYSIS has presented with complaints of
*cough since 20 days
* fever since 20 days
*shortness of breath since 15 days
*decreased urine out put since 3 days.
History of present illness
The patient was apparently asymptomatic 10 years back when he developed throbbing pain in his right metatarso-phalangeal joint, which was associated with swelling and fever. 2 weeks later, he also developed swelling and pain in bilateral knee joints. With these symptoms the patient went to a nearby hospital. On evaluation, he was informed to have increased uric acid (as informed by the attender) and was diagnosed with gouty arthritis; treatment was started for the same (drugs- unknown).
During the same visit he was diagnosed with hypertension and medication was given (Stamlo 2.5mg OD). He has been compliant with the medication till date.
After he was started on medication for the above, he was able to walk for 3 years, following which for next 4 years he used stick to walk. Presently he is able to walk only with the help of a stand.
About since 4 years ago, he developed bowel and bladder incontinence where he was not able to know that he is about to pass stools /urine which is persistent till now.
He discontinued his homeopathic medication from 3 years
His son mentions that since 3-4 years, the patient doesn't recognise family members sometimes and the next day he behaves normally.
Presently, the patient complaints of cough with expectoration since 20 days. Expectoration is mucoid in nature initially he was able to spit out but now removed by suction. He also had complaints of fever with chills from about 20 days with burning micturition.
He also complained of SHORTNESS OF BREATH which was initially of NYHA grade 2 later progressed to grade 4
Then he was taken to a private hospital where they said that he has a kidney problem for which he should undergo dialysis. He was referred to another hospital where he was on dialysis for 5 days and there was no improvement and attender specified that there was no urine output for 2 days during that hospital course. Now the patient was brought to our hospital for dialysis with the above complaints
Past history
* He is a known case of Hypertension since 10 years
* No history of Diabetes mellitus, prior seizures, coronary artery disease tuberculosis, asthma
Personal history
He take a mixed diet, his appetite has decreased since the past 15 days.
He has decreased urine output.
His sleep is disturbed due to cough.
He used to smoke 20 chutas/ day. He started smoking at the age of 17. He stopped smoking 15 years back.
He stopped alcohol intake and smoking about 15 years ago
* Bladder and bowel incontinence since 4 years
Family history
No history of similar complaints in his family
GENERAL PHYSCAL EXAMINATION
*Patient is drowsy
*Not oriented to time and place
*Oriented to person
Patient was moderately built and nourished
He was not able to open his eyes completely
VITALS
* Pulse : 83 beats per minute, regular rhythm , vessel wall was firm in consistency , normal volume and character
* Blood pressure : 110/80 mmHg
*Respiratory rate : 18 cycles per minute
*Temperature ; Afebrile
RESPIRATORY SYSTEM:
INSPECTION:
Chest is symmetrical
Trachea – midline
Apical Impulse : visible
Pectus excavatum : present
no dilated veins, sinuses
no visible pulsations over the chest
PALPATION:
Trachea – midline/shifted
sternum was depressed
dilated veins – not present
Apical impulse : felt at 5th intercostal space 1 cm medial to mid clavicular line
Chest movement : symmentrical
Tactile Fremitus : resonant in all lung fields
PERCUSSION: Dull note in all the lung fields
AUSCULTATION:
1. Breath sounds : Vesicular breath sounds in all lung fields
2. CREPITATIONS were heard all the lung fields
3. supramammary Grunting was present on leftside
4. Vocal fremitus was resonant
CARDIO VASULAR SYSTEM
* Chest is bilaterally symmetrical
* Jvp not raised.
* No precordial bulge
* No parasternal heave
* APICAL IMPULSE WAS SEEN AND FELT OVER 5TH INTERCOASTAL SPACE 1 CM MEDIAL TO MID CLAVICULAR LINE
* On percussion, the heart borders were in normal limits
* On ausultation of the auscultatory areas of heart, S1 S2 Were heard
* No murmurs
CNS
HIGHER MENTAL FUNCTIONS-
Altered sensorium seen
Drowsy and arousable
Speech and language normal
Memory intact
CRANIAL NERVE D-DAY
1, 9,10,11, 12: Could not be elicited due to O2 mask
Other cranial nerves are normal
SENSORY EXAMINATION-
Normal sensations felt in all dermatomes
MOTOR EXAMINATION-
Normal tone in upper and lower limbs
Normal power in upper and lower limbs
REFLEXES-
Normal, brisk reflexes elicited- biceps, triceps, knee and ankle reflexes elicited.
CEREBELLAR FUNCTION-
Normal function
No meningeal signs were elicited.
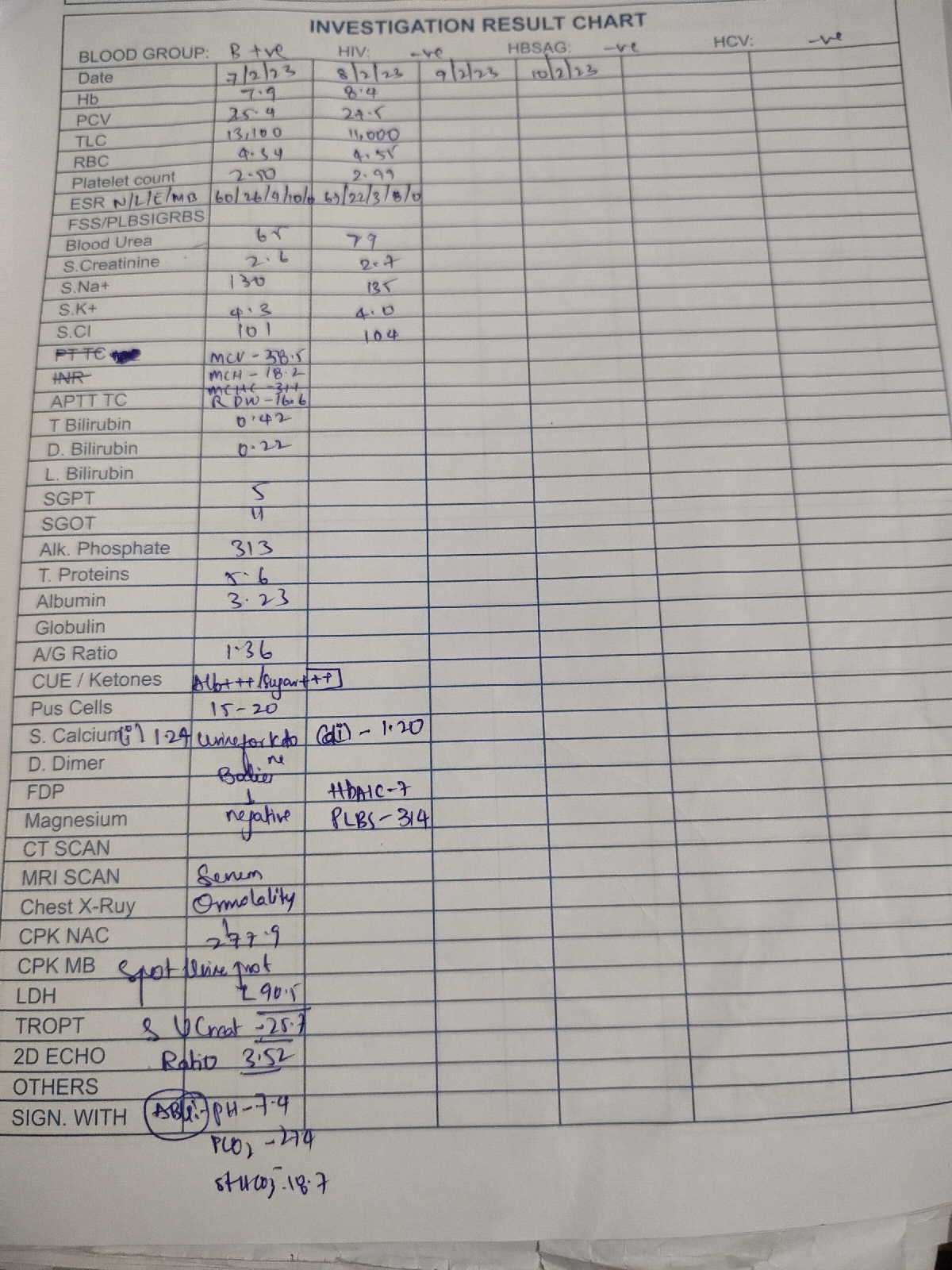
INVESTIGATIONS
LIVER FUNCTION TESTS
BLOOD GROUPING
HEMOGRAM
RENAL FUNCTION TESTS
ABG
ECG
CHEST X RAY
PROVISIONAL DIAGNOSIS:-
ACUTE KIDNEY INJURY ON CHRONIC KIDNEY DISEASE
WITH ASPIRATION
TREATMENT:-
ON 12/1/2021
1. INJ.PAN 40 MG /IV/OD
2. INJ.ZOFER 4 MG /IV/SOS
3. IVF - NS @ UO+50 ML/HR
4. INJ .LASIX 20 MG /IV/BD
5. TAB PCM 650 MG /RT/SOS
6. INJ PIPTAZ 2.25 G /IV/TID
7. BP/PR/TEMP MONITORING 4TH HOURLY
8. GRBS CHARTING 12 TH HOURLY
9. 2nd hourly oral suctioning