case of sob and dysphagia
50 yrs old female patient came with
Chief complaints: sob from 20 days and difficulty in swallowing to solids and liquids from 3 days
And not able to open mouth from 1 day
History of present illness: pt apparently asymptomatic 20 days back and developed sob of grade 2 not associated with orthopnea, pnd ,pedal edema,chest pain, palpitations
From 3 days pt having difficulty in swallowing to solids and liquids and from 1 day not able to open mouth
It is because of reddish discoloration of tongue and pain
History of past illness:
2 months back pt had complaints of cough and expectoration
Pain in chest region went to hospital diagnosed clinically as pulmonary military Tb and started on ATT.
After 1 month she developed redness itching all over body it is ATT induced erythoderma
She stopped ATT (1/2/2022) for 20 days and agin started 1 month back
Know case of
DM 3 months no medication
HTN 10 yrs on medication
TB on ATT. 3 tab per day
She is a know n case of rheumatoid arthritis and hypothyroidism
Personal history
Appetite : normal
diet. : Mixed
Bowel and bladder. Regular
No allergies and no habits
General examination conscious , coherent , cooperative
Pallor present but no
Icterus
Cyanosis
Clubing
Lymphadenopathy
Vitals
BP 130/80mmhg
PR 110 BPM
RR 27
Spo2 95
Systemic examination
CVS
No thrills
S1 S2 heard
No cardiac murmurs
Respiratory examination
Dyspnea present and no wheeze
Position of trachea central
Breath sound s vesicular sounds
Crepts heard at rt infraclavicular area
Abdomen
Soft and non tender
No palpable masses
Liver and spleen not palpable
Bowel sounds heard
No fluid thrills
CNS examination
Higher motor and sensory system were normal
Provisional diagnosis.
Miliary Tb with Att induced erythoderma.
With heart failure . with nutritional anemia
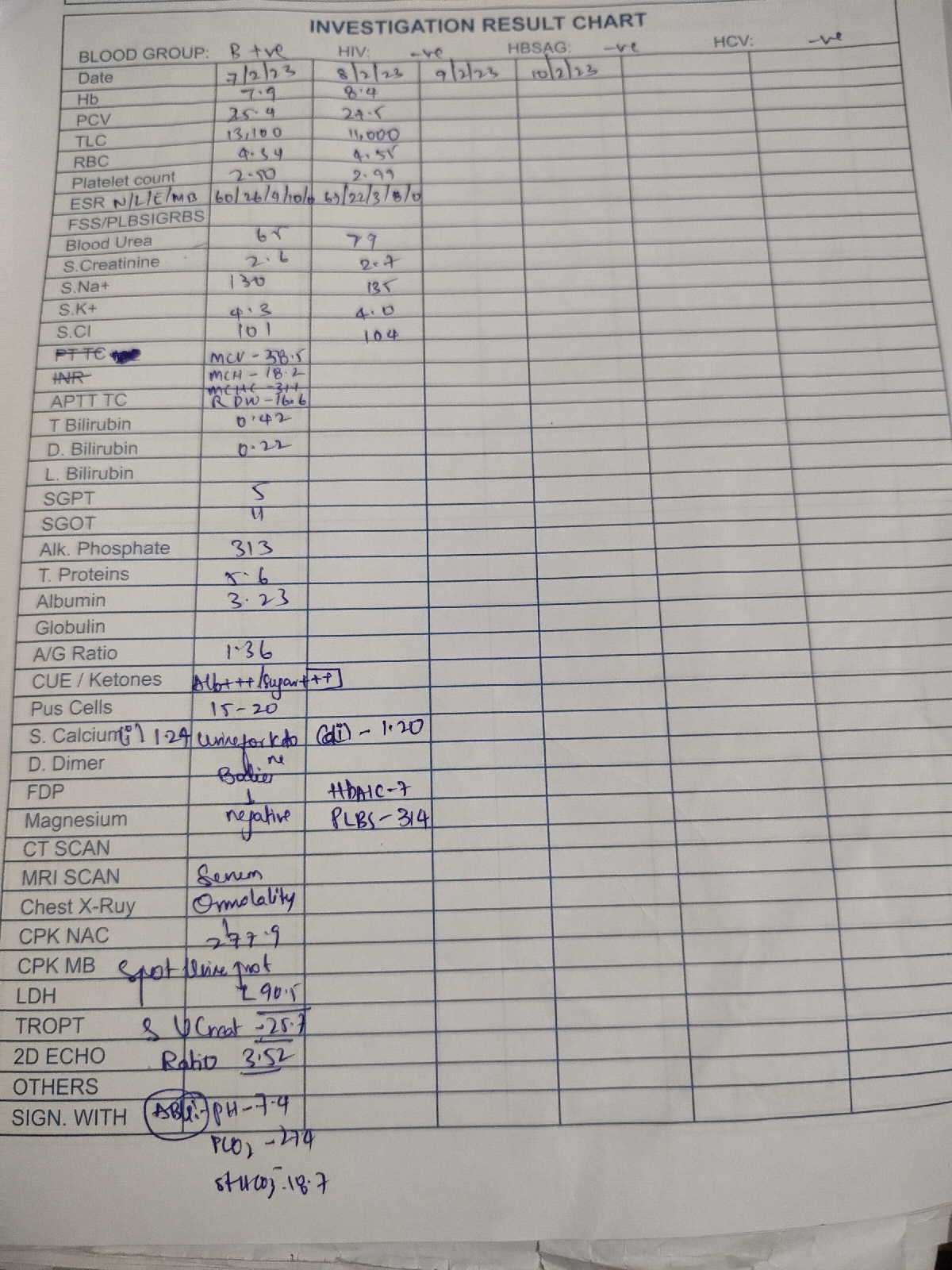
Investigations
USG
1)left mild hydronephrosis
2) mild hepatomegaly with grade 2 fatty liver
X rays
Color Doppler 2D echo
TR and AR
Moderate LV dysfunction
RWMA. +ve with diastolic dysfunction